NHS crisis: Why are so many staff leaving the health service?
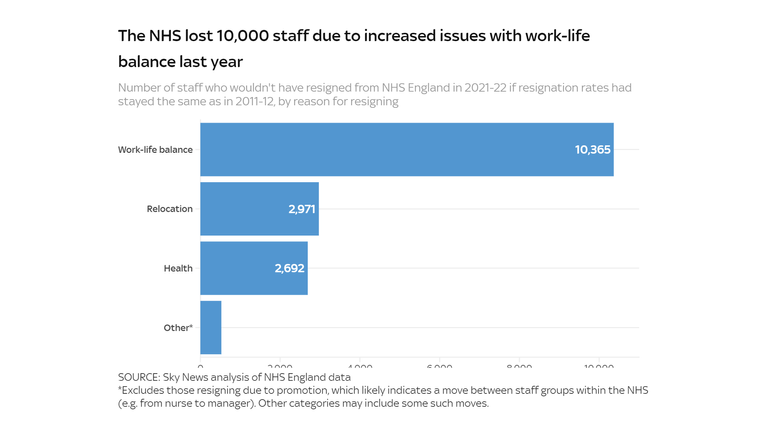
Chronic staff shortages are raising the pressure on NHS staff, with long working hours and high anxiety driving more staff to quit. Sky News analysis shows that a surge in resignations due to work-life balance cost the NHS 10,000 staff last year.
Tuesday 21 February 2023 06:49, UK
In the 24 years Linda Tovey has worked for the NHS, she has never seen the health service so short of staff.
"You’re just not doing the job you signed up for - it’s not possible," the 49-year-old critical care nurse told Sky News.
For the last two years, nurses like Linda have been leaving the health service in record numbers, in part due to the pressures of manning a healthcare system with 133,000 vacant posts. Those that remain are left to pick up the slack.
"You can’t do anything the way you’d want to do it," Linda says. "It’s difficult to say for sure, but there are probably more errors. The idea that it’s less safe for patients causes a huge amount of stress."
Data from NHS Digital shows that 15,000 nurses resigned from the health service in the year to March 2022, with 4,000 citing work-life balance as their reason for leaving.
It’s not just nurses - staff across the NHS are now three times more likely to quit due to issues of work-life balance than they were a decade ago, complicating the health service’s efforts to plug vacancies, expand capacity and bring down waiting lists.
Analysis by Sky News shows that this increase in resignations due to work-life balance cost the NHS 10,000 staff last year. That figure includes 203 doctors, 2,800 nurses and more than 4,100 support staff.
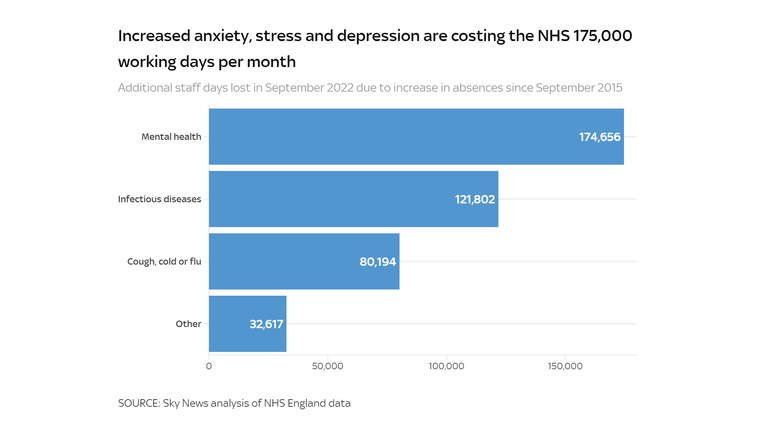
The strain on NHS staff is also evident in the growing number taking time off for mental health reasons. In September 2022, nearly half a million working days were lost to anxiety, stress, or depression-related absences. That's equivalent to one in every 80 working days, a 56% increase since 2015.
Had rates of mental health-related absence not increased since 2015, Sky News analysis has found, the NHS would have had an additional 175,000 working days in September.
On any given day that month, one in every 42 ambulance support staff were absent for mental health reasons, along with one in every 52 midwives.
For doctors in their second foundation year, their first year with a full licence to practice, mental health absences have more than tripled since 2015.
One NHS worker feeling the strain is Kafeelat Adekunle, a 57-year-old community matron.
"If we had enough nurses and they were paid well, no one would be getting stretched or broken," she said. "People wouldn’t be falling sick all the time and leaving the profession."
A recent report by the Institute for Fiscal Studies found that nurses and midwives who took at least three days off for mental health were 27% more likely to have left the NHS altogether three months later. For consultants, the figure was 58%.
It’s not just burnout that's causing staff to leave. Sky News found that a rise in relocation-related resignations cost the NHS nearly 3,000 staff last year.
We don’t know exactly where these staff are relocating to, but data from the General Medical Council (GMC) suggests that many doctors are moving overseas.
Last year, the GMC issued 6,950 certificates of the type typically requested by doctors looking to move abroad. Data from previous years suggests that around half of these doctors are likely to cease practicing in the UK within nine years.
"There’s definitely been a movement of EU nurses back to the EU," says Linda Tovey.
"And other international nurses are going to places where the cost of living crisis doesn’t seem as great. People get paid more in America and Australia."
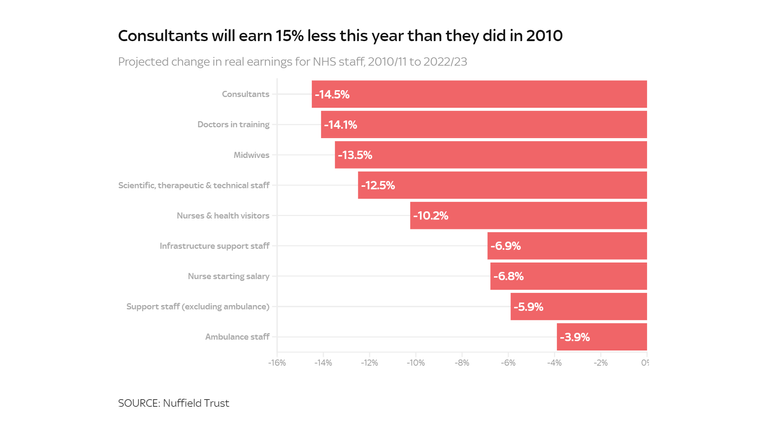
A decade of real-terms pay cuts
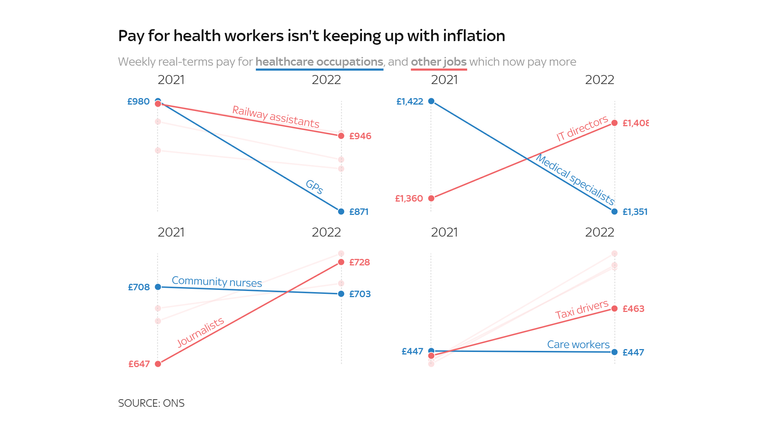
Without an increase in wages, nurses will be paid 10% less in real terms this year than they were in 2010, and consultants 15% less.
"It’s not that doctors in this country are particularly poorly paid compared to other workers," says Billy Palmer, an expert in NHS workforce issues at the Nuffield Trust, a think tank.
"It’s that compared to some high-profile English-speaking countries we lose out. So, it could be quite tempting to go to the US or Australia because you could earn significantly more."
In 2010, a UK medical specialist moving to South Korea would typically see their income fall (in terms of purchasing power) by around 5%, according to OECD data. As of 2020, by contrast, they can expect a pay rise of 25%.
Similarly, a nurse moving to Iceland would previously have taken a 13% pay cut, but is now likely to see a 43% bump to their salary.
Kafeelat Adekunle is among the NHS nurses considering a change of scenery.
"I’m a fighter," she laughs, "but if anything comes up tomorrow I’m ready to go. I have a lot of family in America, and I know I could get more, even double, if I was there today."
The same dynamic is likely to play into foreign healthcare workers’ decisions about relocating to the UK. In 2010, a nurse coming to the UK from Slovenia could expect a 37% boost to their living standards. As of 2020, they would earn 4% more by staying put.
"The international nurses - their expectations are always very high," says Kafeelat. "They’ve given all their savings to escape but now they're earning less, comparably, because of what they have to spend here. It’s a shock.
"One nurse I know has already gone back to Nigeria - she couldn’t cope anymore. I think it was a big shock for her, because she thought she would earn to save. But in this country, you know, you earn to pay your bills."
Fewer EU staff are coming to the UK
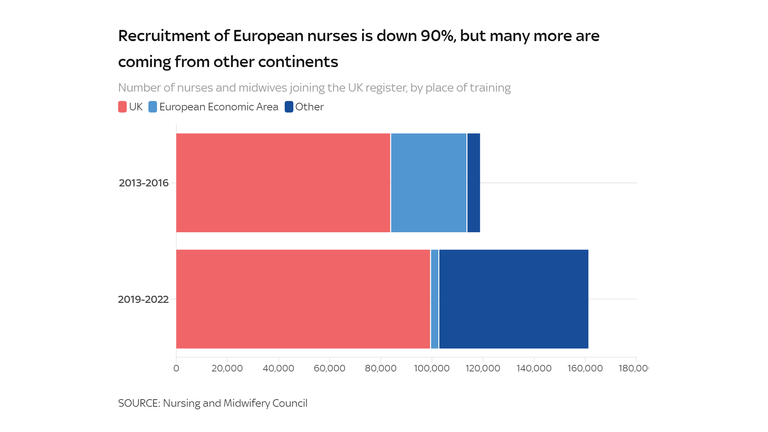
A recent study by the Nuffield Trust found that the number of European health workers moving to the UK has declined steeply since the 2016 Brexit referendum.
Martha McCarey, one of the report's authors, says both pay and a tightening of immigration rules for EU staff are likely to have played a role.
"There's lots of reasons people would want to come to the UK - they might be paid better here than elsewhere, or they're provided with the training opportunities they couldn't have at home. With the current situation, getting better working conditions or pay here might be a less realistic prospect."
The UK recruited 27,000 fewer European nurses during the last four years than it did during the four years before the 2016 Brexit referendum.
Recruitment for nurses from other countries has increased by 53,000 - more than making up the difference.
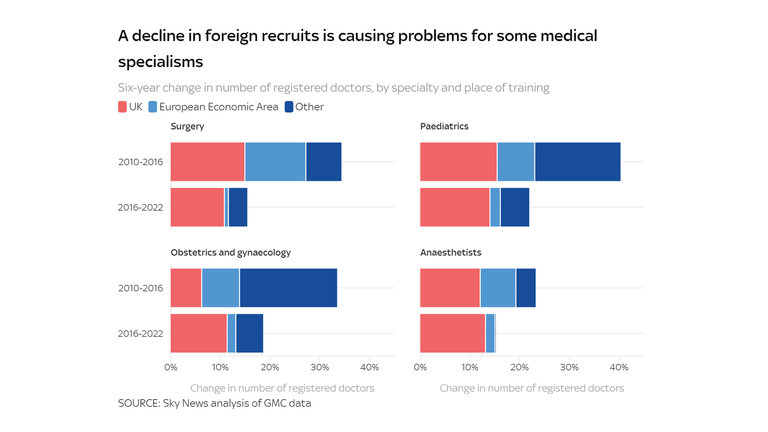
For particular types of doctor, however, that surge in non-European recruitment never happened.
In the six years before the EU referendum, for instance, the number of registered surgeons from outside the European Economic Area (EEA) rose by 861. In the six years since, it has risen by just 726. Combined with a decrease in domestic recruits, that has meant a halving of the growth in the number of surgeons.
The UK relies far more on foreign recruits to staff its health service than other countries. As of 2020, a third of doctors in the UK were trained abroad (32%) - more than double the OECD average of 13%. For nurses the UK is even more of an outlier, sourcing 18% of its staff from abroad compared to an international average of less than 4%.
The UK's reliance on foreign staff is increasing. In 2021, for the first time, doctors from outside the UK or Europe made up the majority of new additions to the medical register.
This could become more of an issue over the coming years, says Martha McCarey, as international competition for doctors and nurses increases.
The World Health Organisation estimates that there will be a global shortage of 18 million healthcare workers by 2030.
The UK’s dependence on foreign staff is also potentially one reason behind the NHS's retention issues.
A recent report by the Institute for Fiscal Studies found that, compared to those trained in the UK, EU-trained consultants were 23% more likely to leave the acute sector in any given month. For those from outside the EU, the difference was 56%.
Growing competition with the private sector
It’s not just other countries that the NHS is competing with for staff, but other sectors within the UK.
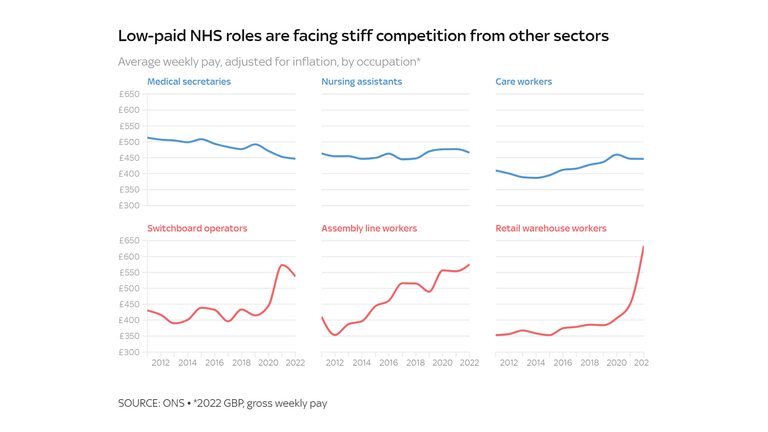
Across the NHS, wages have fallen by 4.6% in real terms since 2010, according to the Nuffield Trust, compared to a 0.6% rise in the private sector. That has put the NHS in direct competition with private employers, particularly for low-paid workers.
It now pays significantly more to be a switchboard operator, assembly line worker or warehouse employee than it does to be a medical secretary, nursing assistant or care worker.
That gap has widened in the last two years, as private-sector employers raised wages to combat their own labour shortages.
Even higher-paying roles, like GPs and specialists, are now facing increased competition from the private sector.
"The feedback you get from junior doctors is that it's pretty toxic working in the NHS at the moment," says Billy Palmer of the Nuffield Trust.
"Feeling valued is important, and a key way people feel valued is through pay. It’s not surprising that people are looking at what other career routes they’ve got."
A "leaky" recruitment pipeline
The government has responded to workforce shortages in part by expanding the number of medical school places, with four new medical schools created between 2019 and 2020.
The increase in medical students has not, however, been matched by a similar increase in training posts, making it harder and harder for trainee doctors to progress.
In 2018, for instance, there were 22,400 applications for 12,400 specialist training posts. By 2022, an increase in the number of medical students meant that the number of applications ballooned to 36,600. The number of posts available, however, shrank to just 12,100. As a result, two in every three applications were rejected (67%) - up from less than half (48%) in 2018.
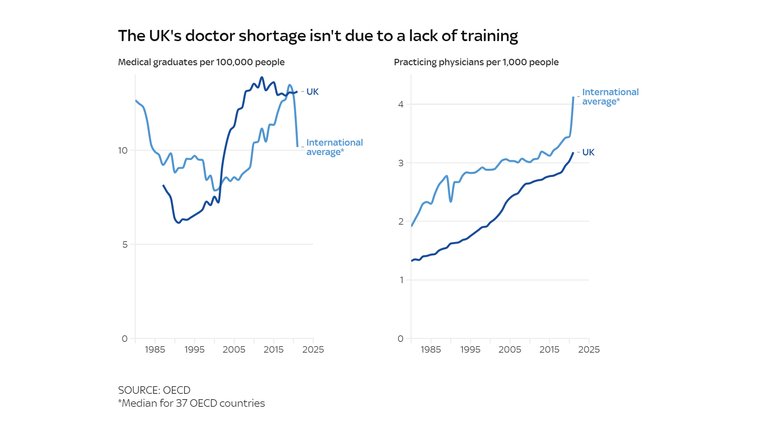
The UK has long struggled to take advantage of its relatively large supply of medical students. For almost all of the last two decades the UK has produced more medical graduates than the average OECD country. Yet for all that time, it has also had relatively few practicing doctors.
"We’ve got a leaky pipe," says Billy Palmer. "It’s not necessarily that we’re not training enough - there’s something happening in that domestic pipeline."
Those issues with career progression, combined with issues around pay and working conditions, are making it difficult for the NHS to retain staff. That, in turn, is hampering the health service's efforts to meet its ambitious recruitment targets.
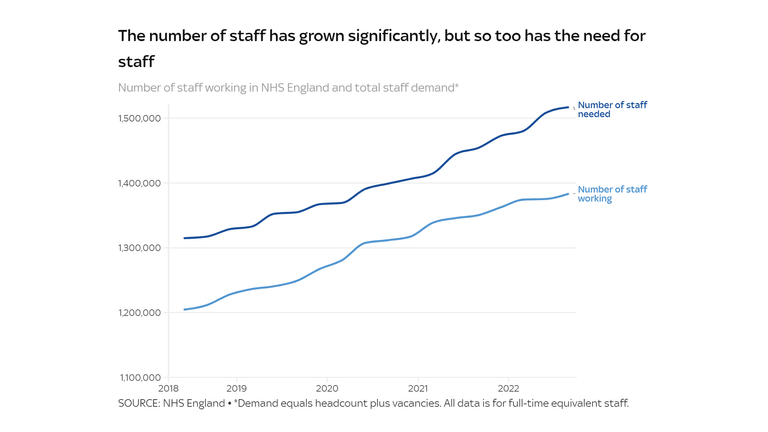
The health service has expanded its workforce by 179,000 in the last four years, but growing demand for staff means that vacancies are rising, not falling.
Billy Palmer says that the NHS has been trying to expand its workforce rapidly in order to boost capacity and reduce waiting lists.
"It’s partly about the amount of activity they’ve got to get through. They’ve got a pretty eye-watering backlog facing them.
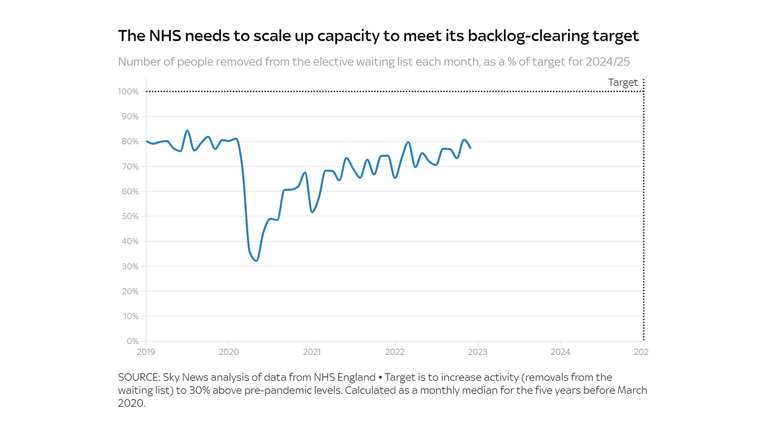
"There’s ambitions to get levels of output to 30% above pre-pandemic levels. Well, how do you go about getting to that? You probably need something like 30% more staff available."
The NHS remains far from meeting that target, and is only just now returning to pre-pandemic levels of elective activity.
Meeting the target is likely to require even more hiring over the coming years. That’s likely to require more funding, but money isn’t the only obstacle.
"You’ve got capacity constraints all along the recruitment path," Billy Palmer says.
"In the education system you need to have classrooms, supervisors, lecturers, accommodation. You also need to have placements in the services. If you’ve got staff in hospitals working flat out, it’s difficult to get them to scale up training."
For experienced nurses like Linda Tovey, higher turnover means more time devoted to training new recruits, adding to the stresses that have been causing the retention crisis in the first place.
"It’s a real strain - you never get a day when someone isn’t following you around. And meanwhile there’s the increasing pressure to carry on, to increase productivity and get everyone through the system."
Strikes feel like "the only way to be heard"
Disputes over pay and working conditions have led to a historic winter of industrial action by NHS staff, including the first-ever strike by the Royal College of Nursing.
Data from NHS England shows that the strikes have resulted in the cancellation of 92,000 appointments since December.
Earlier this month, nearly 50,000 appointments were cancelled in just two days as nurses staged two 12-hour walkouts. The Royal College of Nursing is now preparing to stage its first-ever 48-hour walk-out, from 1 to 3 March.
Kafeelat Adekunle says she joined her local nurses' strike committee because industrial action feels like "the only way to be heard."
"It’s not just the pay, it's the conditions in which we’re working. The government needs to come and shadow some of us. They don’t know what’s happening. They don’t know what we’re going through.
"It’s heartbreaking seeing my profession going down the drain. I've been a nurse forever and I want to be that until I retire.
“We want to do our job, we want to do it right. We want to see our patients, we want to see them well. We want to take care of them. But everyone is exhausted."
The Data and Forensics team is a multi-skilled unit dedicated to providing transparent journalism from Sky News. We gather, analyse and visualise data to tell data-driven stories. We combine traditional reporting skills with advanced analysis of satellite images, social media and other open source information. Through multimedia storytelling we aim to better explain the world while also showing how our journalism is done.